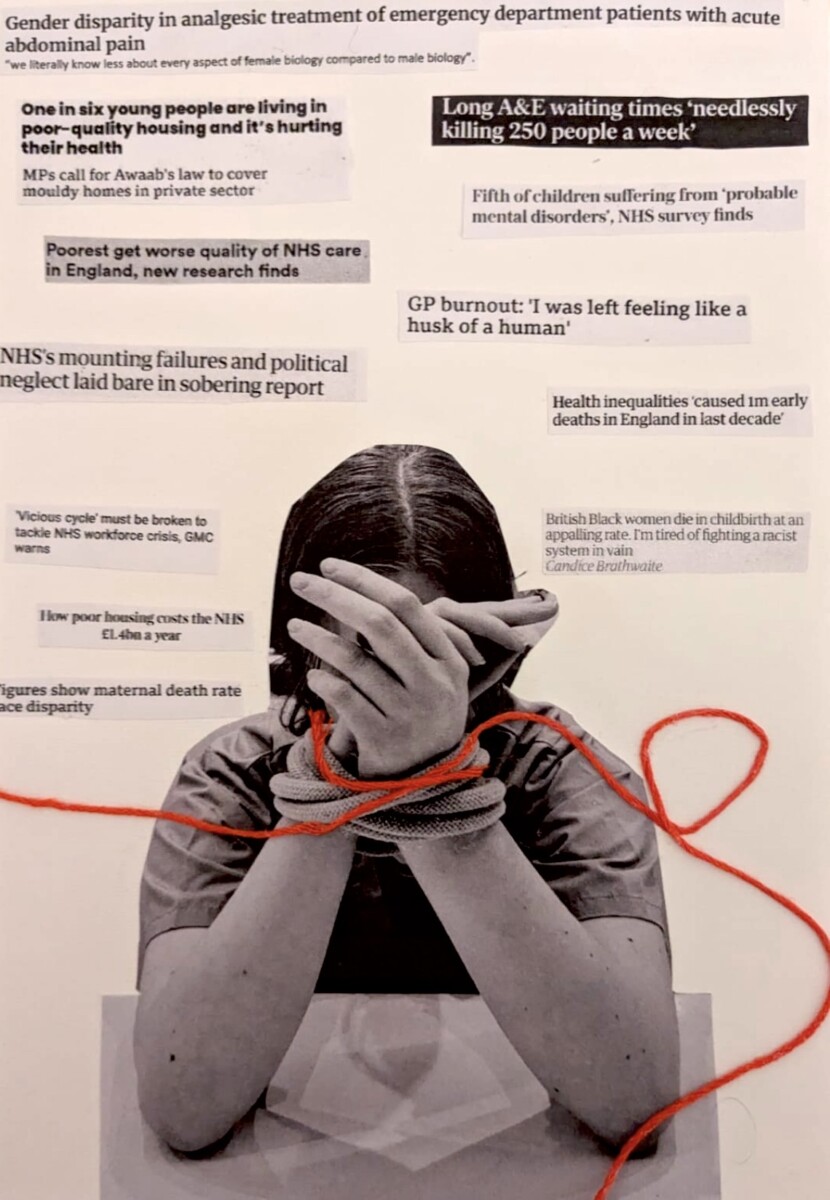
My Hands are Tied
As future doctors we have an inherent desire to heal and make people better, yet throughout my first year of medical school, I have seen first-hand during placements, across hospitals and GPs how much is out of our control.
My art piece shows a doctor whose hands are tied by the various factors that we as individuals cannot change yet have a significant impact on the health and wellbeing of our patients. The headlines surrounding the doctor taken from media articles highlight how the inequality, social and environmental factors I have seen here in Bristol are echoed in hospitals across the country and leave many in our society suffering consequently.
The cost-of-living crisis has left many struggling to make ends meet. It begs the question how we expect our patients to eat healthy food when they rely on foodbanks to feed their family and have little choice on what fills their cupboards each week. How can we help a young child’s respiratory health when they are forced to live in social housing that is damp, mouldy and cold. How can we help patients whose income and employment status already puts them at significantly higher risk of chronic long term physical and mental health problems?
The inequality, prejudice and discrimination experienced by staff and patients motivated by race, gender, social status, medical history or background has catastrophic effects on health both directly and indirectly. Research funding difference, out of date guidelines and archaic hierarchies are just a few roots of inequality, which all result in poorer outcomes for those who need help most. These are systemic failures that have plagued our health service for years, meaning many people are left scared and struggling, unable to get the help they need as we fail to question our own out of date practices, belief and biases.
As clinicians we have to stand back and watch as politicians who have never worked a hospital shift decide how the NHS should be run. We are working in a system that is crumbling around us, surrounded by overworked, underpaid colleagues from every department. As medical students we hear the moans of junior doctors who are placed under huge pressure and expectation, we see the bed-managers frantically trying to place patients in a hospital with inadequate capacity. But you can also feel a huge sense of camaraderie, a sense that we are all in this together and a shared desire to do the best for our patients.
However, when we are doing everything, we can, yet the resources never seem to stretch far enough, it is our patients who must endure the consequences. I have talked to patients who have waited years for a surgery and endured months of pain and discomfort and others who waited hours on a trolly or in an A&E waiting room, just to be seen by a doctor.
Similarly, the increasing demands placed on mental health services mean patients are left to battle with their mental health alone. People are turned away as they are not ‘sick enough’ or don’t meet the criteria to be deserving of help. Our lack of availability means people are forced to reach breaking point before they are seen and tragically this can be too late.
To all these patients and their families all we can say is sorry, there is nothing more we can do in the moment to help. We can offer is a sympathetic ear, maybe a kind smile and sincere apology, but that doesn’t even begin healing the wounds our patients have suffered.
When faced with these systemic, economic, societal and even political problems it can feel like we have failed, despite these all being issues that are beyond our immediate control. It starts to feel that our best is no longer enough.
When presented with the sheer volume out of our control it is easy to despair, yet it really highlights the importance of concentrating on the things we can control:
- We can be compassionate empathetic listeners so our patients can feel safe and validated. They are able to confide in confidence knowing we will do all we can to help.
- We can educate ourselves and our colleagues on disparities and inequalities in healthcare and be aware of our own unconscious biases and actively challenge them each day.
- We can accept and admit ignorance, and we can listen and learn from our patients, colleagues and community to become better able to help and adapt to individual needs.
We can strive to be positive and optimistic in a world that is scary and uncertain.
We will not always be perfect, and the outcome will not always be ideal, but we can support each other through difficult times, accepting what we cannot change and working together to focus on what we can, to create a kinder, more caring and more inclusive health service.
Helen Low, Effective Consulting Year 1, 2023-24
Creative Piece Commended
I enjoyed Helen Low’s portrayal of the common feeling futility of medics because it humanises a misunderstood profession while providing a stark image of the dilemmas many doctors face in their practice. I think public perception of doctors portrays the profession as an elite of highly intelligent and capable individuals who can cure a patient with a touch of their hands or a 10 minute consultation. When a consultation finds no solution or a chronic condition is managed without be cured, this ideal is disabused and the pendulum swings. Medics, or the system they serve, are considered inept and unfit for purpose. They are seen as elites profiting off an image of sanctity they in no way uphold.
The truth is far more nuanced. Medics themselves suffer even more from this idealisation than their patients. In choosing this profession, we see ourselves joining this pantheon of heroes. ‘A crumbling system’ shattered Low’s idea of what it means to be a medic. Scarce resources must be allocated and opportunity costs abound for doctors who truly do want the best for the patients but must face the reality that they cannot always provide it. Low depicts this with a stark red rope – the same colour of the arterial blood that flows from patients waiting to be treated. The pain of being restrained is amplified by the medic’s acute knowledge of the costs of their inaction – lives, pain, families broken. The bowed medic is shown in black and white, drained of the energy that drove them to conquer exams, placements, and endless work to get where they are. The subject is anonymous but is all too well known through the endless flow of articles describing “GP burnout” and “NHS workforce crises.” The piece beautifully and simply captures the public’s view of the NHS as a whole – a failing and unjust system in which Black women die from childbirth at ‘appalling rates’ and inequalities cause millions of deaths.
Medics work for a far-from-perfect system that removes agency from its practitioners. This causes doctors to feel entirely powerless to the realities of a centralised health care project that is underfunded and a society that cannot adequately care for its citizens as a whole. Thankfully, Low’s commentary highlights the ways in which she has been able to focus on the things she can control. Yes we are powerless in some ways but the earlier we understand this, the more we can focus on what we can do and advocate for change in the system we serve. While a bleak picture, Low’s collage is dense with pertinent meaning and stark beauty that can educate patients and practitioners alike.
– The artwork uses an image, real thread and cuttings from real newspaper articles to give the piece a more poignant finish, each element makes it feel that little bit more real and timely, it feels as though you have been projected into the very real emotions of a doctor, the use of black and white was also very tactful, as it symbolises the grey areas in which doctors sit in when dealing with patients and the strains of the NHS. The grey also reflects the mood that surrounds the doctor and the patients which has brought them to this point.
– The artist speaks about how doctors often feel drained and feel as though they have nothing to offer their patients, and speaks about how the challenging circumstances which surround the patient makes them feel helpless and the guilt is overwhelming. The art work itself is named “my hands are tied” this phrase is constantly used in the healthcare profession, and can make not only the doctors and healthcare professionals feel trapped and alone but also the patients. The use of the red string as well as the real rope which was depicted in the image, perhaps symbolises that the greatest barriers of medicine perhaps lie within ourselves and we often can see this invisible red rope tightening around us, this guilt, this feeling of not being good enough is really what is upholding us, the use of red string declares a sense of urgency and pain again tying in with the theme.
– The newspaper articles floating above the persons head perhaps symbolise the overloading worries and pressure, and emphasises how they are always piling on top of us, whilst one may assume that the person in the work is a healthcare worker, it could also be interpreted as a patient, a patient who also feels that their hands have been tied due to the unforeseen circumstances around them