My Pain
The painkillers are pointless.
They make me feel sick,
And drowsy.
The doctor can’t understand.
They make me feel sick,
And drowsy.
The doctor can’t understand.
No one else can feel it,
It is mine, my pain.
It throbs quietly,
And lies in wait.
I can feel it expanding,
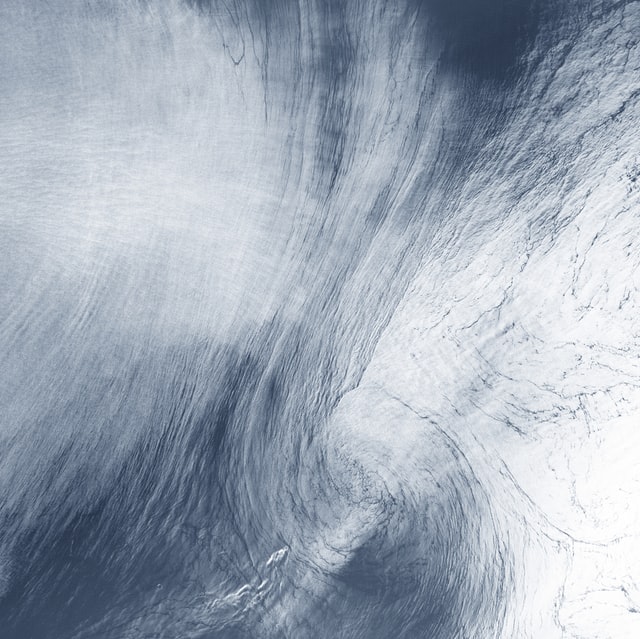
In a wave that moves upwards,
To my throat
Until I can’t breathe.
I fall to the floor,
But don’t notice the crash,
Drop the plate,
But don’t notice the shards.
It passes slowly,
Grip lessening slightly
Until I can see again
Past the darkness.
I stand up again,
Brush up the broken plate,
Throw away the pieces
And sit down.
Wait for the next wave to crash over me.
No one can help me.
I based this poem on one that I wrote during the third session of the course. I found it quite enjoyable to do a creative piece, I think that it is a fairly common problem for patients to believe that a doctor cannot help them – either they don’t trust them or they don’t even think to open up to the doctor about how serious their symptoms are to them. For example, as in this poem, a woman going to a doctor to complain of period pains may receive some painkillers. But if she was to go and complain about how serious it was, the inability to carry out activities as normal for one week out of four, then the doctor may be able to offer further help. This requires a very trusting relationship between patient and doctor and for the doctor to encourage the patient to be open about his or her symptoms. Thinking about this has made me realise the importance of this trust.
Whole Person Care – Year One
I really connected with this piece because even though the writer intended the subject’s pain to have derived from her menstrual cycle, it could be applied to all situations where a patient may be in excruciating pain and yet, doesn’t feel that their doctor empathises with them fully. I interpret the subject’s pain as being psychological or emotional, such as the lowness from being depressed and/or anxious. The subject’s “painkillers” could be any prescribed treatment to help with depression, such as anti-depressants or cognitive behavioural therapy. The subject gives description of ‘being alone’, it’s ‘their pain’, they are ‘in darkness’ and they ‘can’t breathe’ – giving the idea that the patient is very depressed. The last stanza or so is extremely emotive describing how the subject stands up after falling and ‘brushes themselves off’ and waiting for the next time their inevitable pain would return. They feel hopeless and despondent and gears towards the idea that conventional treatment is not right for everyone – every patient is individualistic, and that the subject’s doctor needs to sign-post or find an alternative method to subscribing their subject more ‘painkillers’.