Jane Doe
I chose this perspective as I wanted to put myself in place of a physician and consider how I would delve deeper into a patient’s perspective in order to better understand them, and make connections as to how doing so would help both the quality of healthcare as well as the resilience and wellbeing of the patient. Throughout the piece I also tried to put myself in the shoes of a patient and how I would like to be treated, what questions I would have, and emotions that accompany an illness.
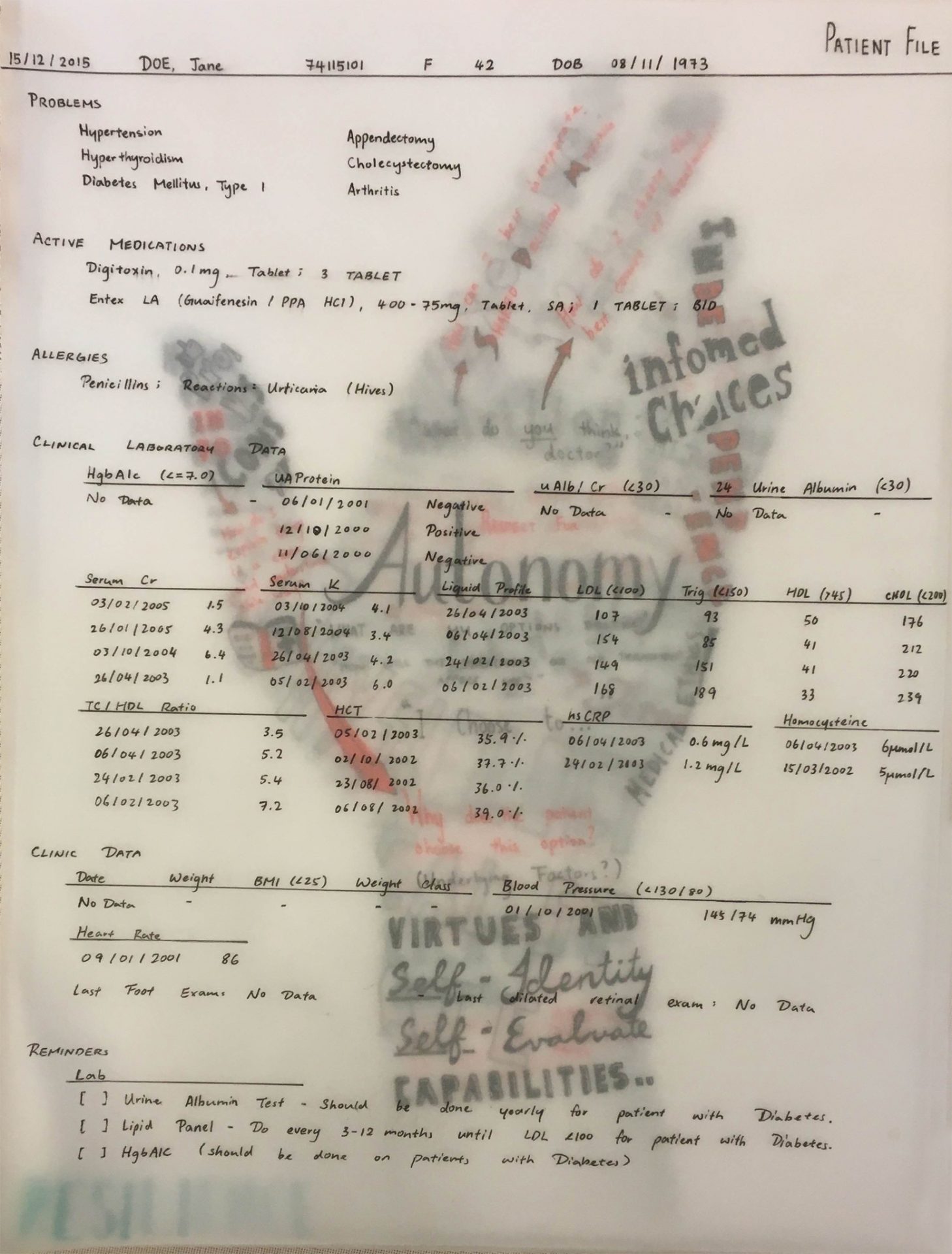
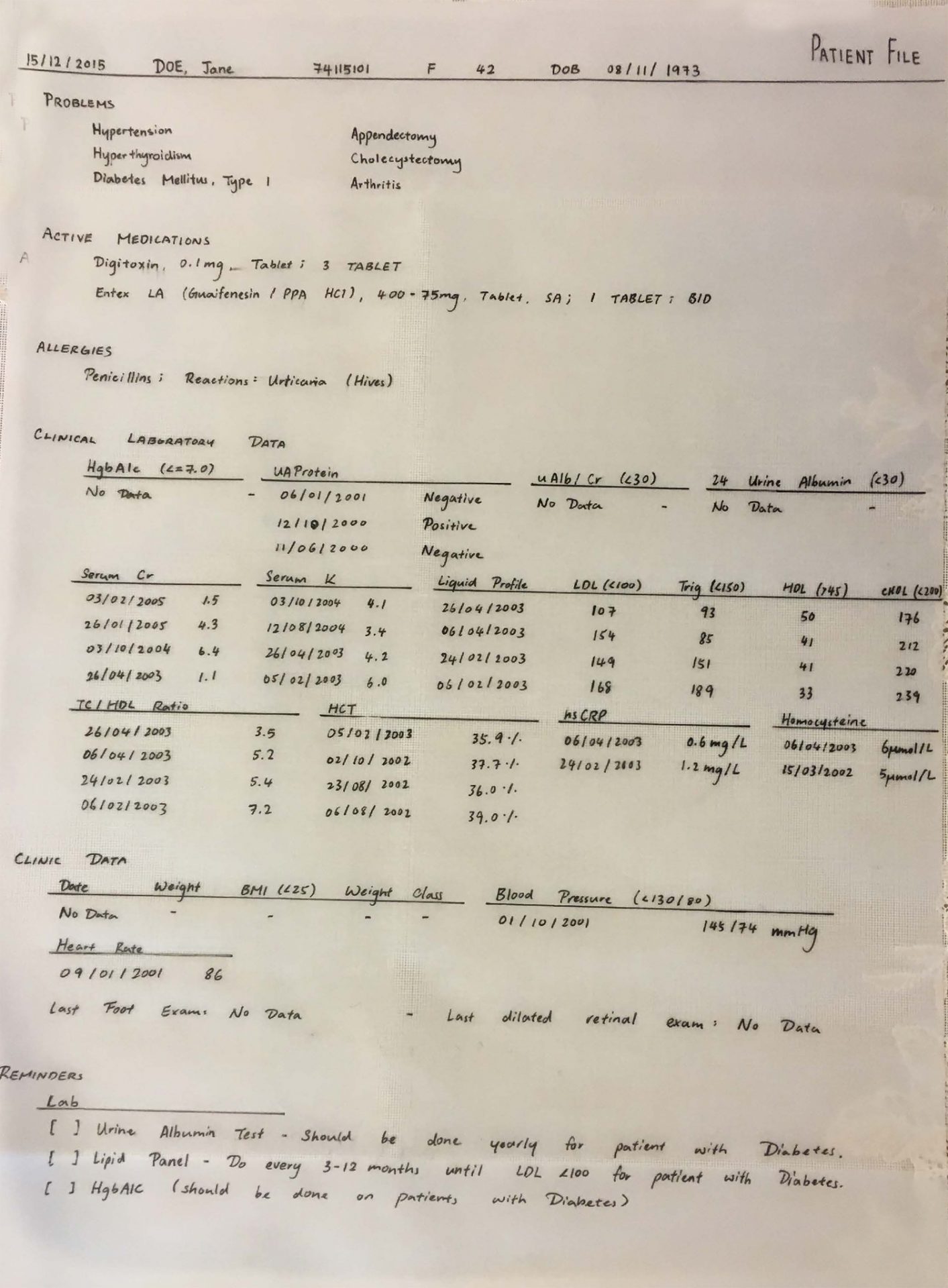
My art piece was constructed of six layers, representing the barriers and stages in consultations in order to find the identity of my patient, from superficial, physical elements to deeper, psychological investigations. I used tracing paper for most layers so that the content beneath would be observable, but only vaguely as would a patient present themselves when they arrive, where their unique stories and substance is hidden and could only be guessed at, but they are definitely there.
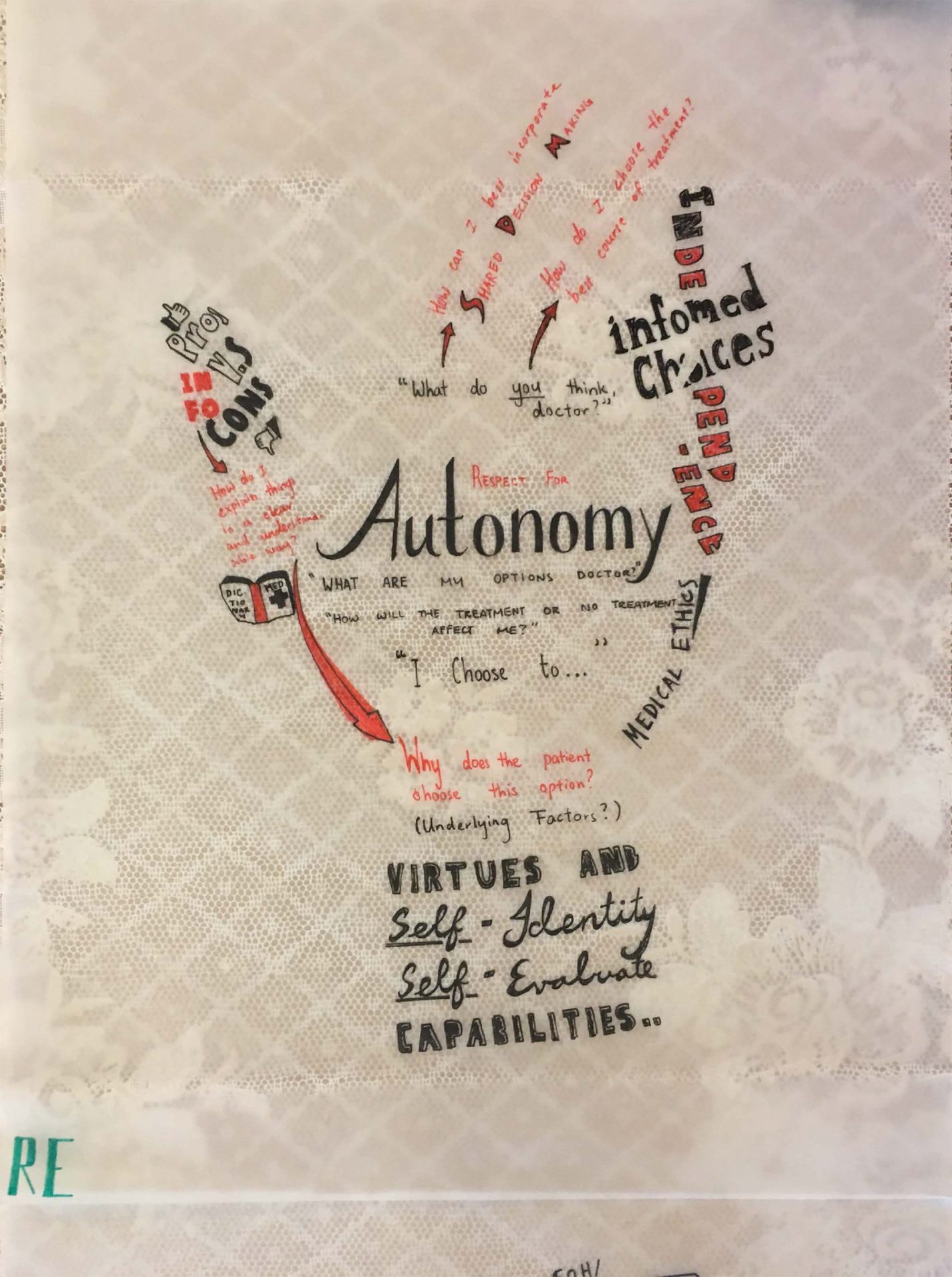
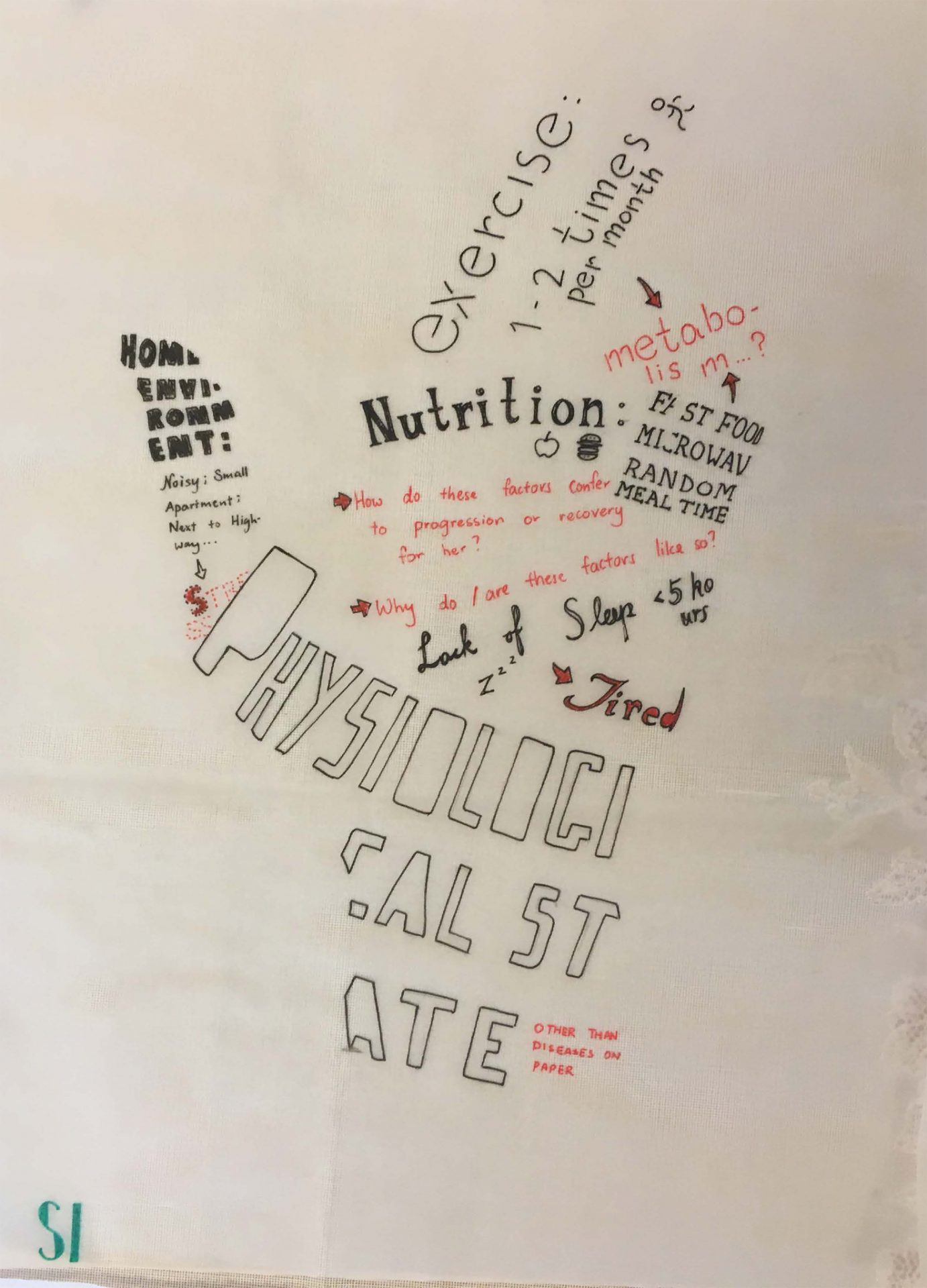
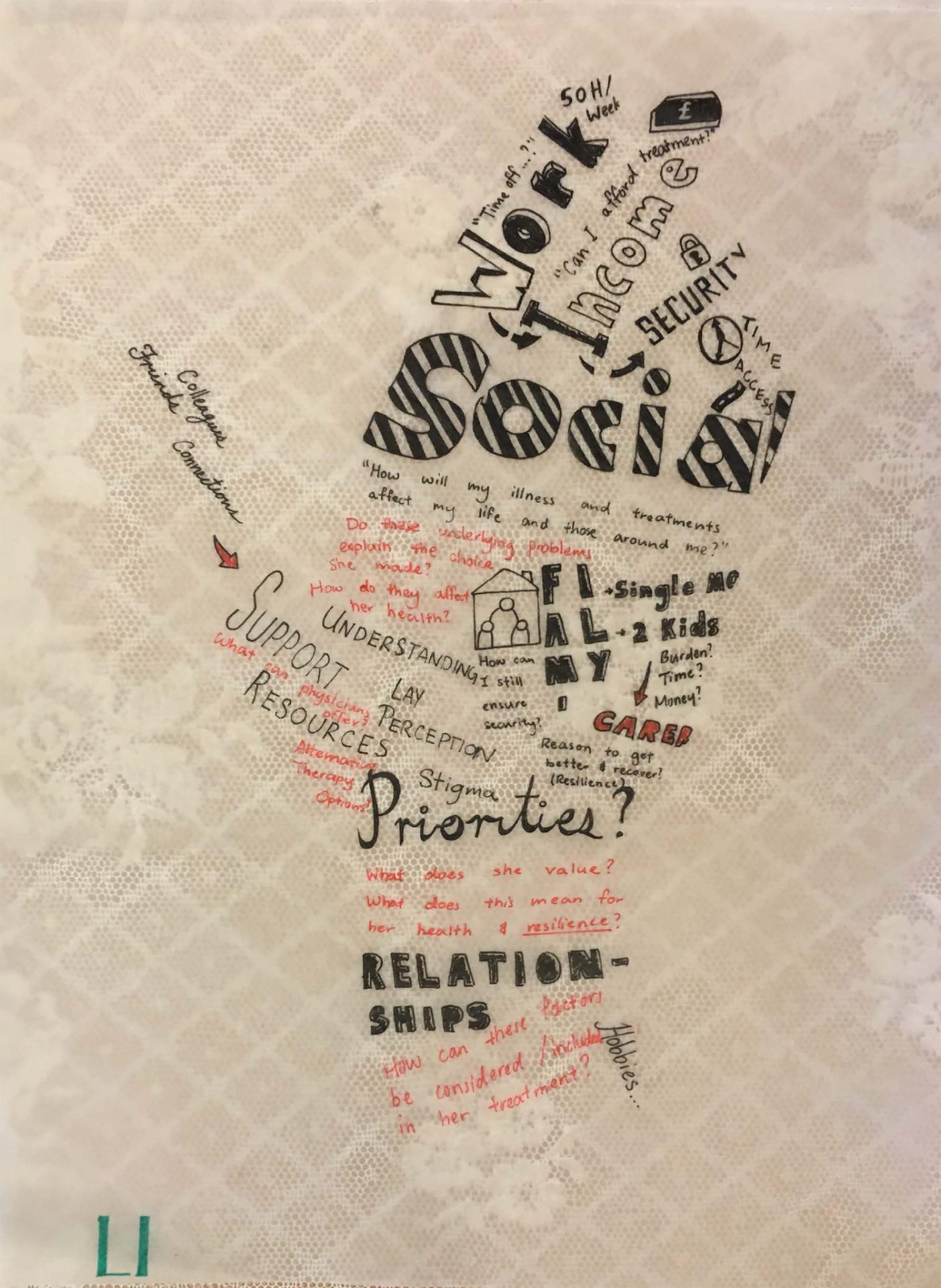
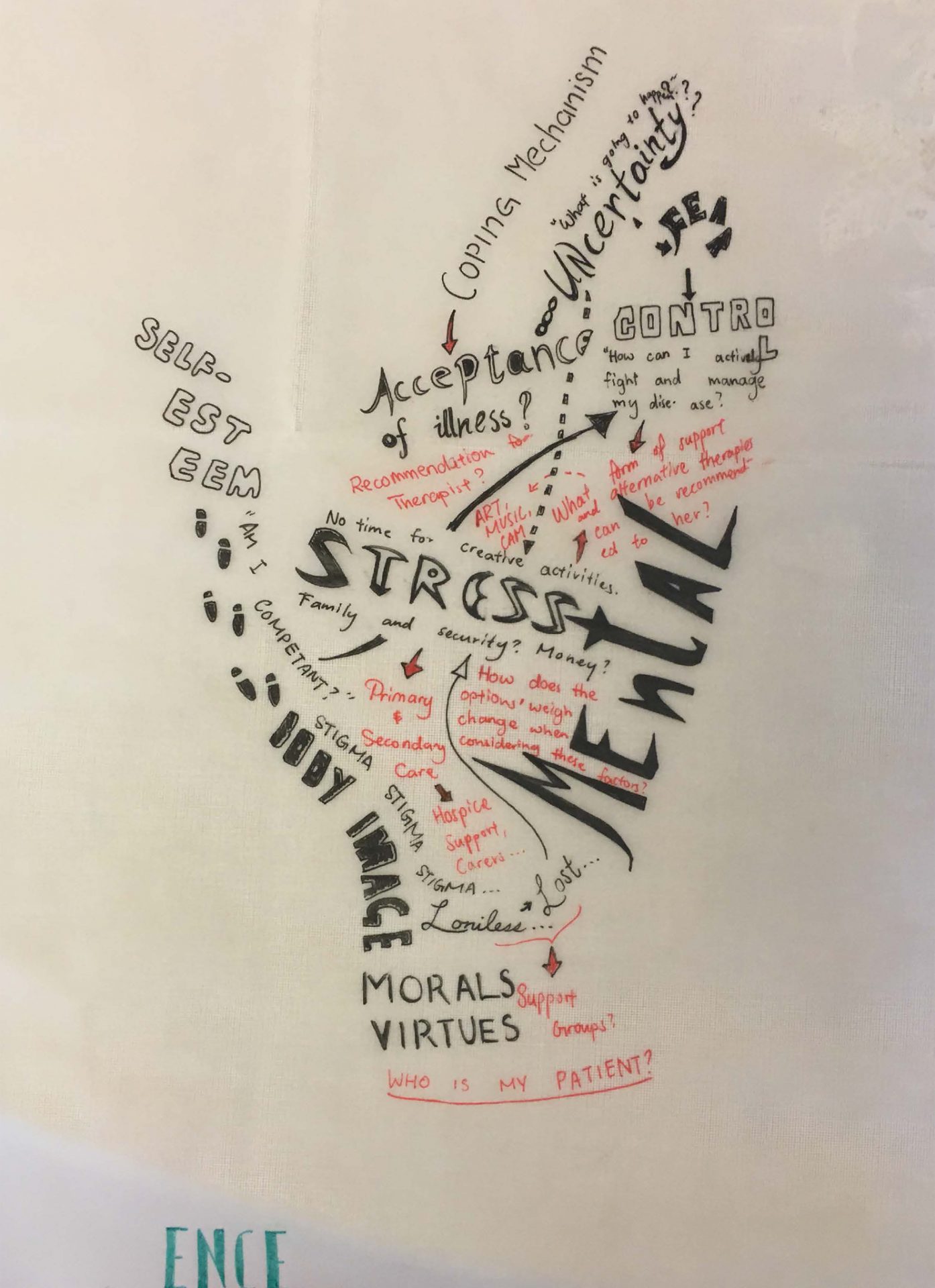
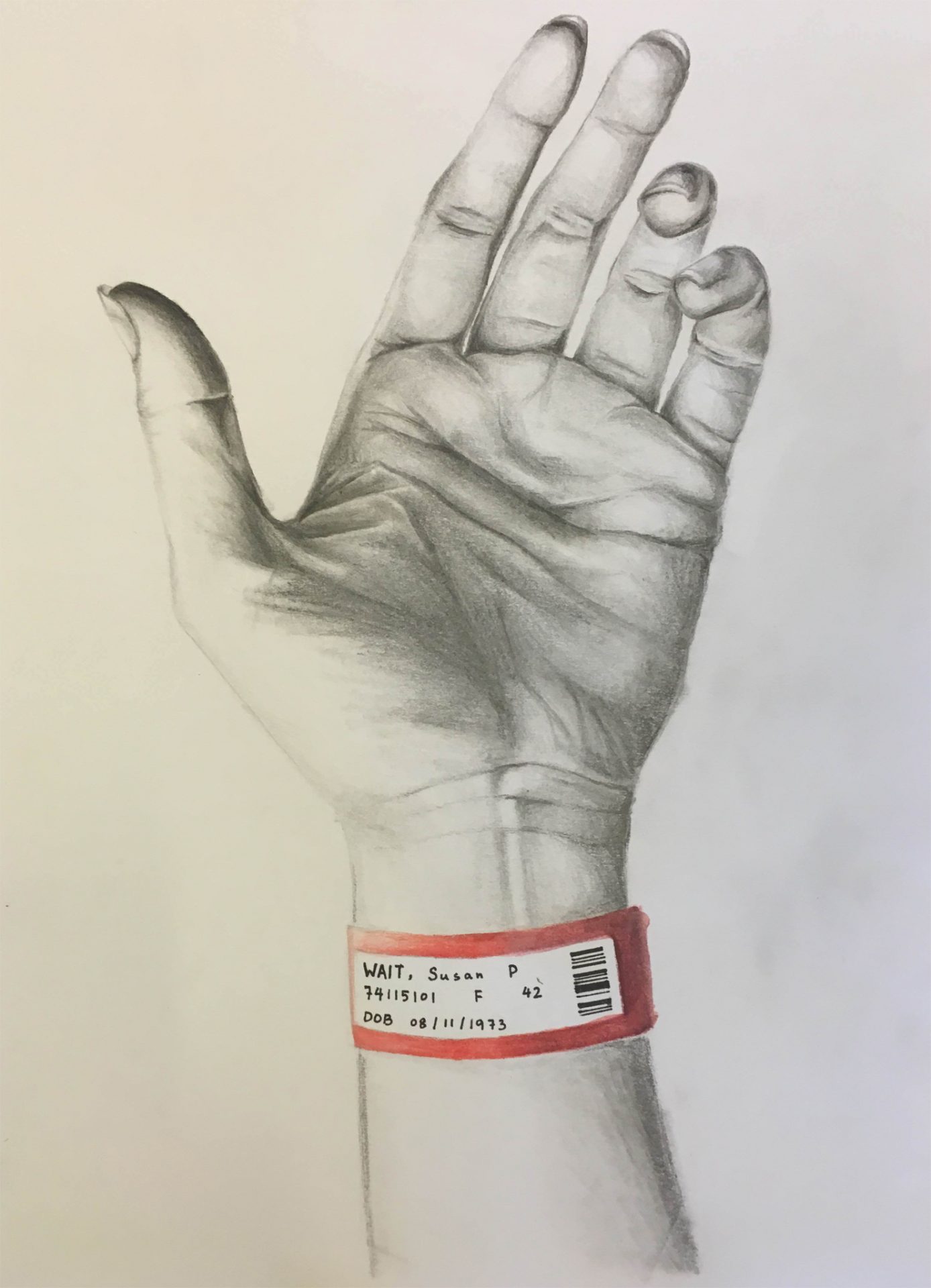
The first layer is a medical report, which listed quantitative data = diseases of the patient, medications, history, laboratory data the bulk of which would be the first thing physicians usually comes across when they encounter the patient. However, these physical categories are very superficial and tell nothing about the patient as an individual. To emphasise this, the name of the patient is written as the generic JANE DOE although there is detailed data about the patient’s physical health, their identity is unknown. When a healthcare professional is willing to communicate and look beyond their own agenda towards the patient’s priorities, they start to discover more about them and compile information which makes up the patient’s resilience. This is shown by the keyword ‘RESILIENCE’ being separated onto all the sheets so it can be seen when they are stacked together. The individual layers all contain a large theme: Autonomy, Physiological State, Social, and Mental. I tried to choose these themes based on Maslow’s hierarchy as well as the order in which they are revealed. Autonomy is the first layer because the first revealing clue about a patient’s identity lies in their choices, which should emerge from the clues given in previous layers, a compilation of mental characteristics, worries, and other concerns are revealed. The layers get progressively more filled up as the doctor begins to understand the patient more, and more links are made (shown by arrows) and they feel respected by medical practitioner. From there, an examination of the patient’s physiological health (including exercise, nutrition, rest etcetera) reveals any contributing factors to their illness. A further investigation prompts elements that make up the patient’s social circle and worries, and begins to reveal a lot more about them as individuals. Finally, the bottom layer shows a realistic drawing of the patient’s hand with a hospital tag that had a name on it, representing the discovery of the patient’s identity and hence seeing a real rather than generic person.
On each layer, I used distinctive black and red ink pens to represent the thoughts and possible dialogues of both the patient (black) and clinician (red). The idea was that I would brainstorm whatever came to mind if I was in either’s shoes and write down relevant keywords regarding the main theme of the layer. This was very enlightening and I gradually became more involved and absorbed as I went deeper. Other than being able to see how these layers are interconnected, I found it easier to draw links between the doctor and patient dialogues, as if I was practicing communicating with a patient in this fashion in my head. The concept of resilient systems and how they are formed in people also became much clearer after this activity with each layer I was able to consider and draw in more factors that could play a role in not only someone’s physical health, but also their mental health. When I finished all the layers with tracing paper, I could truly appreciate the realism and blank page of the patient’s hand, as if I finally discovered the reason behind drawing it in the first place.
However, one thing I noted was that the entire process was very time consuming, not in terms of drawing everything, but in terms of brainstorming different possible factors that could affect a patient’s health and resilience. This made me question the practicality of making such detailed connections with patients within the short consultation time frame in healthcare systems in response to the influx of people waiting to be treated. The current NHS policy of 10-15 minute consultations would barely be enough to scrape past one personal problem, let alone multiple layers and yet, if each patient was allocated the time to express all their wishes, the healthcare system would be entirely over stressed by the amount of work that would need to be done. This is a precarious balance that needs to be further examined for the best quality of care and an efficient system.
Ultimately, healthcare extends beyond simply treating the patient for a disease it is also about management of illness and promoting metaphysical wellbeing as a whole. It is no longer adequate to only consider the physician’s agenda, which places a focus on the physical disease and neglects hidden worries, concerns, and feelings of patients. As a result, this paternalistic relationship between doctors and patients leads to a dysfunctional and unsatisfactory outcome that discourages resilience and positivity in shared decision-making. However, when patients autonomy is respected and their agenda more understood in integrative medicine, their self-identities, self-evaluations, and capabilities are better valued, this not only enables the quality of healthcare to be improved and suited to the individual, resilience in patients can also be enhanced by recommended therapies that tackle the root of their problems, contributing to improving their overall health.
Reference
1. Entwistle VA, Carter SM, Cribb A, McCaffery K. Supporting Patient Autonomy: the importance of clinician-patient relationships. Journal of General Internal Medicine. 2010 Jul 1;25(7):741-5.
0 Comments